Acne - short tutorial
Acne
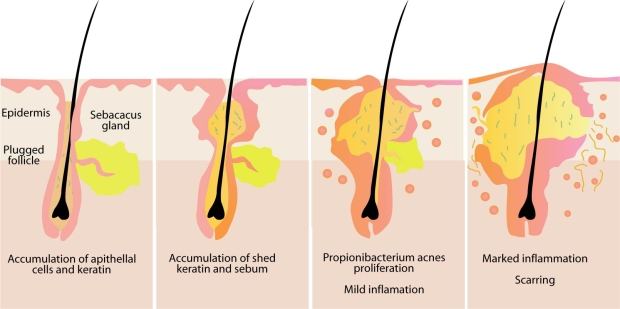
Acne (full name: Acne vulgaris) is a skin disease caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland).
Severe acne is inflammatory, but acne can also manifest in non inflammatory forms.
Acne lesions are commonly referred to as pimples, spots, or zits.
Acne is most common during adolescence, affecting more than 85% of teenagers, and frequently continues into adulthood. For most people, acne diminishes over time and tends to disappear or at the very least decrease after one reaches his or her early twenties.
The face and upper neck are the most commonly affected, but the chest, back and shoulders may have acne as well.
Typical acne lesions are comedones, inflammatory papules, pustules and nodules. Some of the large nodules were previously called "cysts" and the term nodulocystic has been used to describe severe cases of inflammatory acne.
Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated by some to lessen the overall impact to individuals.
What causes acne ?
Acne develops as a result of blockages in follicles. Hyperkeratinization and formation of a plug of keratin and sebum (a microcomedo) is the earliest change. Enlargement of sebaceous glands and an increase in sebum production occur with increased androgen (DHEA-S) production at adrenarche. The microcomedo may enlarge to form an open comedo (blackhead) or closed comedo (whitehead). Whiteheads are the direct result of skin pores becoming clogged with sebum, a naturally occurring oil, and dead skin cells. In these conditions the naturally occurring largely commensal bacteria Propionibacterium acnes can cause inflammation, leading to inflammatory lesions (papules, infected pustules, or nodules) in the dermis around the microcomedo or comedo, which results in redness and may result in scarring or hyperpigmentation.
Primary causes
Several factors are known to be linked to acne:
Hormonal activity, such as menstrual cycles and puberty. During puberty, an increase in male sex hormones called androgens cause the glands to get larger and make more sebum.
Inflammation, skin irritation or scratching of any sort will activate inflammation. Anti-inflammatories (a class of drugs used to reduce inflamation) are known to improve acne.
Stress, through increased output of hormones from the adrenal (stress) glands.
Hyperactive sebaceous glands, secondary to the above mentioned hormone sources.
Accumulation of dead skin cells.
Bacteria in the pores. Propionibacterium acnes (P. acnes) is the anaerobic bacterium that causes acne. In-vitro resistance of P. acnes to commonly used antibiotics has been increasing.
Use of Anabolic steroids.
Any medication containing lithium, barbiturates or androgens.
Exposure to certain chemical compounds. Chloracne is particularly linked to toxic exposure to dioxins, namely Chlorinated dioxins.
Exposure to halogens. Halogen acne is linked to exposure to halogens (e.g. iodides, chlorides, bromides).
Several hormones have been linked to acne: the androgens testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), as well as insulin-like growth factor 1 (IGF-I). In addition, acne-prone skin has been shown to be insulin resistant.
Treatments
In general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
1. Normalising dead cell shedding into the pore to prevent blockage.
2. Killing P. acnes using anti-biotics.
3. Using drugs with anti-inflammatory effects.
4. Hormonal manipulation to balance Androgens and adrenaline hormone activity.
A combination of treatments can greatly reduce the amount and severity of acne in many cases.
Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of expert supervision.